Vertebral Body Tethering – VBT

What is VBT?
Vertebral Body Tethering, or VBT for short is the newest surgical treatment available for treating scoliosis. The surgery was developed in the United States of America approximately 10 years ago by a group of US spinal surgeons.
The surgery is minimally invasive in comparison to the more traditional method of fusion although this is still a highly invasive procedure.

How is VBT Performed?
VBT is carried out anteriorly (through the side). Incisions are made under the arm to perform the surgery and an endoscope is used removing the need to have an open back incision.

1 week, 2 months, 6 months scars post VBT
Titanium pedicle screws are anchored into each of the vertebrae making up the curve and a flexible Polyethylene-terphthalate cord is then attached to each screw and tightened to pull the spine straight. Where patients have remaining growth the tether is tensioned accordingly allowing the spine to grow in length normally whilst allowing for additional straightening of the spine until the adolescent finishes growing.
Where patients have a c shaped curve a single tether is fitted and with an s shaped curve a double tether is inserted, one tether for each curve.
Who is a Candidate for VBT?
Previously VBT was only suitable for children with remaining growth and curves between 40 and 70 degrees. In more recent years the technique has been adapted for use with older teens and in a small handful of cases adults.
In all cases spine flexibility is key to being a candidate.
Whilst there are several surgeons throughout the world now performing this procedure each surgeon has their own criteria and parameters within which they work. More information on this can found in the two support groups.
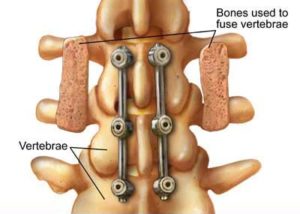
Advantages of VBT over Fusion
- Surgery is less invasive. Performed endoscopically meaning little or no blood transfusion needed and less risk of infection.
- Faster recovery due to less muscle, bone, tendon and tissue damage.
- No intersegmental fusion.
- The spine is able to continue growing in length due to the flexible tether.
- Patient retains full flexibility of the spine in all direction.
- Normally back to full activities within 6 weeks.
- No bridges burned. In the unlikely event of a complication other procedures such as fusion can still be carried out in the future.
Complications
Over Correction
Overcorrection can be thought of as too much of a good thing. The scoliosis corrected beyond straight and started curving in the opposite direction from the original curve.
Surgeons use the Risser and Sanders scores to estimate how much growth a child has left when planning for surgery. Based on these scores and family height patterns, the surgeon makes a decision about how close to a “straight” correction to achieve at the time of surgery. If a child has an estimated large amount of spinal growing left to do, caution is taken to reserve some curvature to allow them to grow out of the remaining curve on their own. That is called growth modulation. In more mature adolescents who are nearly finished growing, the goal is to get as much correction as possible at the time of surgery.
Overcorrection happens when the adolescent grows much more than expected and the cord is now tighter on that side than it needs to be. More growth remaining = more risk of overcorrection and less growth remaining = less risk of overcorrection There is no “formula” or absolute way to prevent potential for overcorrection in immature spines, but that is where the knowledge and experience of the surgeon is paramount. (On the flip side, If too much slack is left in the cord to accommodate a lot of anticipated growth, and that growth does not happen, the spine will not growth modulate and the curve will “under correct”.)
The surgeon will monitor for signs of overcorrection on subsequent x-rays and may describe the (Cobb angle) curves as a “minus # degrees”. Some overcorrection is acceptable, especially if it is not noticeable and the adolescent is finished growing. Fortunately, overcorrection is not that common. But if significant overcorrection does occur, several surgeons have good experience revising these cases without fusion. Recovery and return to activity is quicker than the original surgery.
Cord Breakage
In very rare instances the cord can break if under too much tension. When the tether breaks it breaks between the two vertebrae leaving the remainder of the spine tethered. A watch and wait approach would normally be adopted before a decision is made as to whether additional surgery to correct the breakage is needed.
